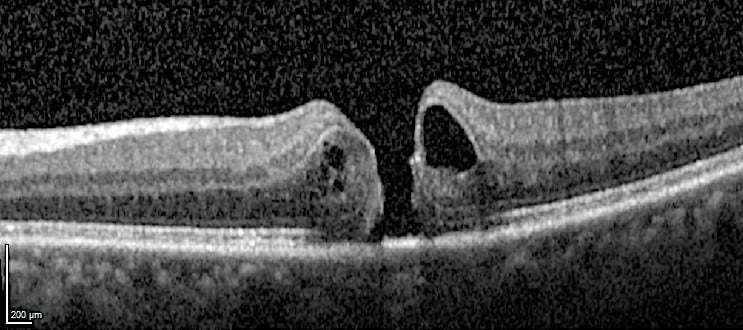
The exact pathogenesis of macular holes is unknown, but in most cases they are thought to be caused by vitreous traction avulsing macular tissue. The resulting full-thickness defect is usually centred on the fovea. This produces a central visual defect with blurred vision and distortion.
OCT showing a full-thickness hole in the centre of the macula (the fovea).
Normal OCT.
Treatment
Without treatment only a small minority of macular holes resolve and treatment is usually recommended. However, if the macular hole has been present for a long time, the chance of closure is much lower and the decision to treat needs to be carefully balanced.
Usual treatment is with surgery – a pars plana vitrectomy, internal limiting membrane (ILM) peel and intravitreal gas injection. Surgery leads to macular hole closure in 80-90% of eyes. Not all eyes with hole closure have visual improvement, but most do. However, fully normal vision is seldom achieved.
Referral guidelines
Macular holes are treated by vitreoretinal surgeons. Please refer within one month.
Further information about macular holes and their treatment can be found in our patient information leaflet.