Retinal detachment usually occurs when a posterior vitreous detachment pulls a break in the retina, and vitreous fluid passes into the potential space between the retina and retinal pigment epithelium (RPE).
The detached retina does not see, so the patient experiences an enlarging visual field defect. If the detachment extends to involve the macular (a macula-off retinal detachment), then visual acuity drops precipitously.
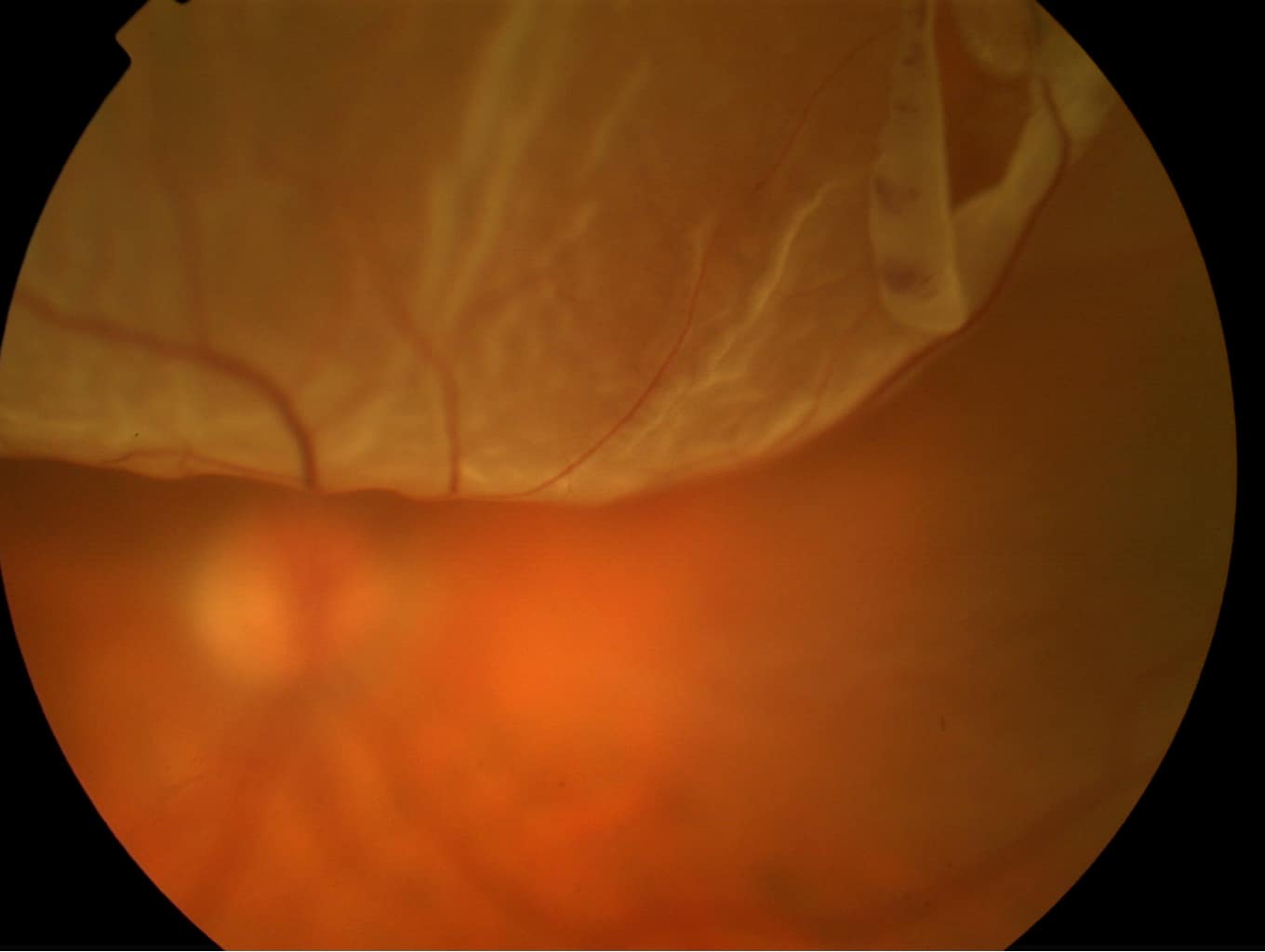
Fundus photo of a superior retinal detachment caused by a large horseshoe-shaped retinal tear seen top right.
Occasionally, retinal detachments are asymptomatic, but the characteristic symptoms are easily remembered as FFF:
- Field defect (often experienced as a dark veil starting in the peripheral vision)
- Flashing lights (photopsia)
- Floaters in the vision
Treatment
Treatment involves one of three strategies:
- pneumatic retinopexy
- cryobuckle surgery, or
- pars plana vitrectomy with laser and/or cryotherapy and gas tamponade.
All involve retinopexy, whereby laser or a cryoprobe is applied to the causative break in the retina, to seal the defect.
Pneumatic retinopexy is reserved for a small number of straightforward detachments; it has the advantage that it is a simple procedure, but it has a fairly high failure rate, with about 30% of cases going on to require cryobuckle or vitrectomy. It involves an intravitreal gas injection and cryotherapy or laser to the breaks.
Cryobuckle involves the use of scleral explants to indent the sclera/RPE in apposition to the retina.
Vitrectomy involves removal of the vitreous gel, which is replaced with a slowly absorbing gas bubble. Most retinal detachments are treated by vitrectomy, cryotherapy and gas.
Because of the gas bubble, patients have certain restrictions after surgery including the need to position their head, restrictions on flying/altitude and avoidance of some inhalational anaesthetics, until the gas is reabsorbed.
Occasionally, chronic, stable retinal detachments can be observed.
Referral Guidelines
Occasionally, asymptomatic, chronic retinal detachments are detected during routine optician examination and can be referred semi-urgently (1-2 weeks). However, in all other situations please refer patients the same-day, or first thing next morning if presenting late in the evening.
Further information about retinal detachment and its treatment can be found in the following patient information leaflet.